
Introduction
A blood clot is a mass of blood that forms when platelets, proteins, and cells in the blood stick together. While clotting is essential to stop bleeding from injuries, clots that form inside veins or arteries without injury can be dangerous. These clots can block blood flow, leading to serious health problems like strokes, heart attacks, or deep vein thrombosis (DVT).
Understanding how to avoid blood clots is essential because early prevention can reduce the risk of life-threatening complications. Clots can develop without warning, making it vital to recognize risks and take proactive steps to prevent them.
Certain groups face a higher risk of developing clots. People who are immobile for long periods, pregnant women, older adults, smokers, and those with medical conditions like cancer or heart disease are more vulnerable. This guide aims to help anyone who might be at risk understand how to reduce their chances of developing a clot and stay healthy.
What Are Blood Clots?
A blood clot is your body’s natural way of stopping bleeding when you get injured. It forms when platelets, proteins, and cells in your blood clump together, creating a plug that seals wounds and prevents excessive blood loss. This process, known as clotting, is essential for healing.
However, not all clots are helpful. While normal clotting happens at the site of an injury, harmful clots can develop inside veins or arteries without any external wound. These clots can block blood flow, leading to serious health issues.
What causes blood clots to become dangerous often comes down to their location and movement. A clot that forms in a deep vein, like in the leg, is known as deep vein thrombosis (DVT).
If part of this clot breaks off and travels to the lungs, it can cause a life-threatening condition called a pulmonary embolism. Similarly, clots in arteries can block blood flow to the heart or brain, resulting in heart attacks or strokes.
Understanding the difference between normal and harmful clotting is vital. While your body needs clots to heal wounds, clots that form without injury or don’t dissolve properly can pose serious health risks. Recognizing these risks is the first step toward protecting yourself from complications.
What Causes Blood Clots?
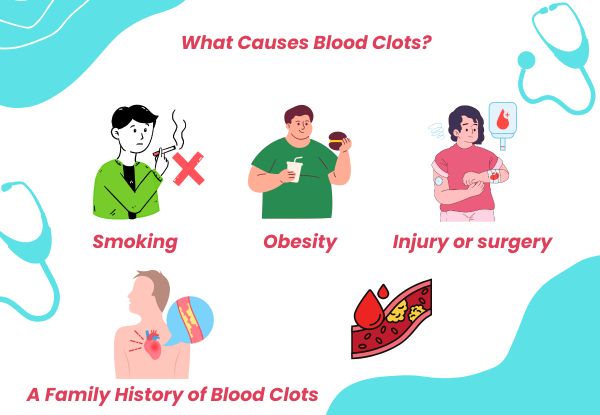
Understanding what causes blood clots is essential to preventing them. Clots can form due to several factors, some related to lifestyle and others to underlying health conditions.
1. Prolonged Inactivity:
Sitting or lying down for long periods slows blood flow, increasing the risk of clots. Long flights, extended hospital stays, or working at a desk without moving around can lead to blood clot formation, especially in the legs.
2. Surgery or Injury:
Surgical procedures, especially those involving the hips or legs, can damage blood vessels, triggering clot formation. Post-surgery immobility also increases the risk. Injuries that cause blood vessel damage can lead to a clot as part of the body’s natural healing process.
3. Certain Medications:
Some medications, like hormone replacement therapy or birth control pills, can increase clotting risk. These drugs may alter blood composition, making it more likely for clots to form.
4. Health Conditions:
Certain medical conditions heighten the risk of clots:
- Deep Vein Thrombosis (DVT): A serious condition where a clot forms in a deep vein, usually in the leg. DVT Treatment in Mumbai provided by specialists like Dr Chandrakant focuses on managing and preventing complications such as pulmonary embolism.
- Heart Disease: Conditions affecting the heart and blood vessels can cause clots to form in arteries, leading to heart attacks or strokes.
- Cancer: Some cancers and their treatments can increase the risk of blood clots.
- Obesity and Diabetes: These conditions can lead to poor circulation and changes in blood composition, making clotting more likely.
5. Other Risk Factors:
- Smoking: Damages blood vessels and affects clotting.
- Pregnancy: Increases pressure on veins and changes blood flow, raising clot risk.
- Genetics: A family history of blood clotting disorders can make some people more susceptible.
Recognizing the reasons for blood clots helps in taking the right preventive measures. Early detection and appropriate treatment, especially for conditions like DVT, are essential to avoid severe complications.
Who Is at Risk of Developing Blood Clots?

While blood clots can affect anyone, certain people face a higher risk due to specific health conditions, lifestyle factors, and situations that slow or alter blood flow. Understanding these risk factors is essential to preventing problems related to blood clotting.
1. Risk Factors That Increase Blood Clot Risk:
- Age: As people get older, especially over 60, the risk of blood clots increases due to slower blood circulation and age-related health issues.
- Obesity: Carrying extra weight can put pressure on veins, particularly in the lower body, slowing blood flow and raising the chance of a clot.
- Smoking: Tobacco damages blood vessels, making them more prone to forming clots and contributing to problems related to blood clotting.
- Pregnancy: Blood flow changes during pregnancy, and increased pressure on the veins in the pelvis and legs can lead to clot formation.
- Cancer: Some cancers and their treatments can make the blood more likely to clot.
- Genetic Conditions: Inherited disorders can increase clotting tendencies, even without obvious risk factors.
2. High-Risk Scenarios for Blood Clots:
- Post-Surgery: Surgery, particularly orthopedic procedures like hip or knee replacements, can damage blood vessels and reduce mobility, increasing clot risk.
- Long Flights or Car Rides: Sitting for long periods without moving can slow blood flow in the legs, leading to clot formation.
- Extended Bed Rest: Whether due to illness, injury, or recovery, staying in bed for long periods reduces circulation, which can result in blood clots.
- Trauma or Injury: Broken bones, muscle injuries, or severe bruising can lead to clots, especially in deep veins.
3. Medical Conditions That Raise Clot Risk:
- Heart Disease: Conditions that affect blood circulation can increase clotting risk.
- Diabetes: High blood sugar levels can damage blood vessels, contributing to clot formation.
- Autoimmune Disorders: Diseases like lupus or antiphospholipid syndrome can make the blood more likely to clot.
Recognizing who is at risk allows for proactive steps to reduce the chance of blood clots. For individuals facing multiple risk factors, speaking to a healthcare professional can help create a prevention plan tailored to their needs.
Symptoms of Blood Clots You Shouldn’t Ignore

Recognizing clot symptoms early can make a significant difference in preventing serious health complications. Blood clots can develop in various parts of the body, and their symptoms depend on where the clot forms. Some clots, like those resulting from an injury, may be less dangerous, but others can be life-threatening if left untreated.
1. Blood Clots in the Legs (Deep Vein Thrombosis – DVT):
Clots in deep veins, typically in the legs, are known as DVT. Common symptoms include:
- Swelling in the leg, usually on one side.
- Pain or tenderness that starts in the calf and feels like cramping.
- Warmth around the swollen area.
- Skin discoloration, turning red or bluish.
These clot symptoms should not be ignored, as DVT can lead to serious complications if the blood clot travels to the lungs.
2. Blood Clots in the Lungs (Pulmonary Embolism – PE):
A PE happens when a blood clot breaks off from another part of the body (often the legs) and lodges in the lungs. This can be life-threatening. Symptoms include:
- Sudden shortness of breath.
- Sharp chest pain that worsens with deep breaths.
- Rapid heartbeat or irregular heart rhythms.
- Coughing, sometimes producing blood.
If you notice these symptoms, immediate medical attention is necessary.
3. Blood Clots in the Brain:
A clot in the brain can lead to a stroke. Common symptoms include:
- Sudden weakness or numbness on one side of the face or body.
- Trouble speaking or understanding speech.
- Severe headache without a clear cause.
- Loss of vision in one or both eyes.
- Difficulty walking or loss of balance.
4. Blood Clot from Injury:
Not all blood clots are harmful. After an injury, the body naturally forms a clot to stop bleeding. However, in some cases, these clots can migrate or grow, leading to complications. If swelling, redness, or pain increases around an injured area, it’s important to seek medical advice.
When to Seek Medical Help:
If you notice any of these clot symptoms, it’s essential to get diagnosed quickly. Facilities like the Best diagnostic center in Mumbai can perform tests such as ultrasounds and blood tests to confirm the presence of a blood clot. Timely diagnosis can prevent life-threatening complications like PE or stroke.
Knowing the signs and acting fast can save lives. Never ignore sudden changes in your body that could indicate a blood clot, especially if you have existing risk factors.
How to Avoid Blood Clots: Prevention Strategies

Preventing blood clots starts with understanding how daily habits impact your risk. Learning how to avoid blood clots is essential, especially for people who may already be at a higher risk. Simple lifestyle changes, dietary choices, and medical support can go a long way in reducing the chances of clot formation.
Stay Active and Move Regularly
One of the most effective ways to reduce the risk of blood clots is staying active. Regular movement keeps blood flowing smoothly and helps prevent pooling, especially in the legs.
- Why Movement Matters:
Inactivity slows blood circulation, increasing the risk of clots. This is why learning how to prevent blood clots starts with staying physically active. - Tips for Staying Active:
- For frequent travelers on long flights or road trips, standing up and walking every hour can help. Simple calf exercises, like ankle rolls or foot flexes, also improve circulation.
- Desk workers should make it a habit to stand up and stretch every 30 minutes. A short walk or leg stretches under the desk can prevent blood pooling.
- Incorporating light exercises such as walking, swimming, or yoga into your routine improves circulation and strengthens the veins.
By staying active, you’re taking an important step in how to avoid blood clots and improve your overall health.
Healthy Diet and Hydration
The food you eat and how hydrated you are play a role in blood flow and clot prevention. Certain foods can naturally thin the blood and support circulation.
- Best Foods to Prevent Blood Clots:
- Leafy greens like spinach and kale provide nutrients that support healthy blood flow.
- Berries contain antioxidants that help maintain healthy blood vessels.
- Garlic and onions are natural blood thinners, promoting smoother circulation.
- Omega-3-rich foods like salmon and flaxseeds help reduce inflammation and improve blood flow.
- The Role of Hydration:
Dehydration thickens the blood, increasing the risk of clots. Drinking enough water throughout the day ensures proper blood consistency and flow.
A balanced diet combined with good hydration can make a significant difference in reducing your risk of blood clots.
Medical Prevention Methods
In some cases, lifestyle changes alone may not be enough. Medical treatments can offer additional protection, especially for those at higher risk.
- Blood Thinners:
Medications prescribed by a doctor can help prevent clots, especially for individuals who have already had a blood clot or are at high risk. - Compression Stockings:
These specially designed stockings apply gentle pressure to the legs, promoting blood flow and preventing clots, particularly useful for those recovering from surgery or long periods of immobility. - Regular Blood Tests:
A blood test for blood clots can help identify clotting issues early. Regular testing is essential for individuals on blood thinners or those with clotting disorders. - Expert Consultation:
Consulting a DVT Treatment Specialist can provide a personalized prevention plan, especially if you’ve had a blood clot in the past or have multiple risk factors.
Lifestyle Changes to Lower Risk
Certain lifestyle habits directly impact clotting risk. Making positive changes can significantly reduce your chances of developing a blood clot.
- Maintain a Healthy Weight:
Excess weight puts additional pressure on veins, increasing the risk of clots. A balanced diet combined with regular exercise can help manage weight effectively. - Quit Smoking:
Smoking damages blood vessels and promotes clot formation. Quitting reduces this risk significantly and improves overall vascular health. - Limit Alcohol Consumption:
Drinking too much alcohol can lead to dehydration and poor circulation, both of which contribute to blood clot risk. Moderation is key.
Adopting these lifestyle changes is one of the most effective ways to prevent blood clots and improve long-term health.
How to Detect Blood Clots Early
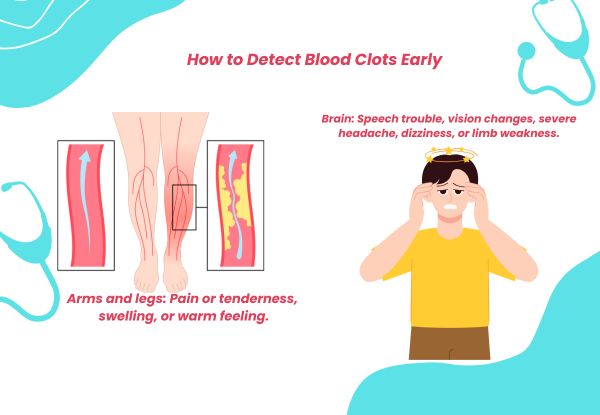
Early detection of blood clots can prevent life-threatening complications. Many clots develop silently, without immediate symptoms, making it important to recognize warning signs and undergo timely medical tests. If you have risk factors or a history of clotting, regular screening can help identify issues before they become serious.
Common Diagnostic Methods
Medical professionals use several tests to confirm the presence of a blood clot. These tests help determine whether a clot is forming, where it is located, and if immediate treatment is needed.
- Ultrasound:
This is the most commonly used test to check for blood clots in deep veins, especially in the legs. A Doppler ultrasound can measure blood flow and detect abnormalities that may indicate a clot. - Blood Test for Blood Clots (D-Dimer Test):
This test measures D-dimer levels, a substance released when a blood clot breaks down. High levels may suggest clot formation, though additional tests are often required to confirm. - CT or MRI Scans:
For suspected clots in the lungs or brain, imaging tests such as CT pulmonary angiography or MRI venography provide detailed insights into blood flow and blockages. - Venography:
In some cases, a contrast dye is injected into a vein to create clearer X-ray images of the blood vessels, helping detect blockages caused by blood clots.
Importance of Regular Check-Ups
Regular check-ups play a vital role in detecting blood clots early, especially for those at higher risk. If you have a history of blood clotting disorders, are on blood-thinning medications, or have recently undergone surgery, routine screenings can help prevent complications.
- People with deep vein thrombosis (DVT) history should have regular follow-ups to monitor circulation.
- Individuals on medications that affect clotting should undergo periodic blood tests for blood clots to assess treatment effectiveness.
- Those with lifestyle risk factors, such as prolonged inactivity, obesity, or smoking, should consult a doctor about preventive screenings.
Early detection increases the chances of effective treatment and lowers the risk of complications such as pulmonary embolism or stroke. Staying aware of symptoms and seeking medical attention at the first sign of a blood clot can make a significant difference in overall health.
Treatment Options for Blood Clots
Understanding how to cure blood clots is essential for preventing serious complications. The right treatment depends on the blood clot’s location, size, and potential risks. Early medical intervention increases the chances of a full recovery and reduces the risk of long-term issues.
Anticoagulants (Blood Thinners)
Anticoagulants are the most common treatment for blood clots. These medications help prevent existing clots from growing and reduce the risk of new clots forming.
- Types of Anticoagulants:
- Heparin: Often administered through an IV or injection for rapid action, especially in hospital settings.
- Warfarin: An oral blood thinner that requires regular monitoring through blood tests to ensure proper dosage.
- Direct Oral Anticoagulants (DOACs): Medications like rivaroxaban and apixaban that offer effective blood thinning without frequent monitoring.
- When Anticoagulants Are Used:
These are typically prescribed for conditions like deep vein thrombosis (DVT) or pulmonary embolism (PE). Anticoagulants are also used preventively after surgeries to reduce clot risk.
Thrombolytics (Clot-Busting Medications)
In more severe cases, thrombolytics may be necessary. These powerful medications actively dissolve blood clots and restore normal blood flow.
- When Thrombolytics Are Used:
Thrombolytics are usually reserved for life-threatening situations, such as a large clot in the lungs or brain, where rapid treatment is critical. - How They Work:
Administered through an IV, thrombolytics work quickly to break down the clot, but they also come with a higher risk of bleeding, making close medical supervision essential.
Surgical Interventions
In certain cases, surgery may be the best option for curing blood clots, especially when medications aren’t effective or when a clot poses an immediate threat.
- Thrombectomy:
A surgical procedure where the blood clot is physically removed from the vein or artery using specialized tools. - Inferior Vena Cava (IVC) Filter:
For individuals who cannot take blood thinners, an IVC filter may be placed in a large vein to catch clots before they reach the lungs. - Catheter-Directed Thrombolysis:
A minimally invasive procedure where a catheter delivers clot-busting medication directly to the blood clot site.
Tailoring Treatment to the Patient
At Midas Care Clinic, specialists assess each case individually to recommend the most effective treatment plan. Factors like the clot’s location, size, and the patient’s overall health influence the choice of therapy.
- For DVT in the leg: Anticoagulants and compression stockings are often used.
- For PE in the lungs: A combination of thrombolytics and anticoagulants may be necessary.
- For clots in the brain: Immediate intervention with thrombolytics or surgical options can prevent strokes.
Understanding how to cure blood clots starts with proper medical guidance. Whether through medications, minimally invasive procedures, or surgery, personalized care ensures the safest and most effective outcomes. Always consult healthcare professionals, like those at Midas Care Clinic, for accurate diagnosis and tailored treatment options.
Complications If Blood Clots Are Left Untreated
Ignoring a blood clot can lead to serious health issues. When a clot blocks blood flow, it can damage organs and lead to life-threatening complications. Understanding the potential risks highlights why early detection and treatment are essential.
Pulmonary Embolism (PE)
One of the most dangerous outcomes of an untreated blood clot is a pulmonary embolism. This happens when a clot, often from the leg (deep vein thrombosis or DVT), travels to the lungs and blocks a pulmonary artery.
- Symptoms of PE:
- Sudden shortness of breath
- Sharp chest pain, especially when breathing deeply
- Rapid heart rate
- Coughing, sometimes with blood
A PE can quickly become life-threatening if not treated promptly, making it one of the most severe problems related to blood clotting.
Stroke
A blood clot that travels to the brain can block an artery, leading to a stroke. This cuts off oxygen to parts of the brain, potentially causing long-term damage.
- Signs of Stroke:
- Sudden numbness or weakness, especially on one side of the body
- Trouble speaking or understanding speech
- Loss of vision in one or both eyes
- Severe headache with no known cause
Strokes caused by blood clots require immediate medical attention to prevent lasting disability or death.
Deep Vein Thrombosis (DVT) and Post-Thrombotic Syndrome (PTS)
When a blood clot forms in a deep vein, usually in the leg, it can lead to DVT. Without treatment, DVT can cause long-term complications like post-thrombotic syndrome.
- Symptoms of PTS:
- Persistent leg pain and swelling
- Skin discoloration
- Development of ulcers near the affected vein
PTS can impact mobility and quality of life, making it another serious problem related to blood clotting.
Chronic Venous Insufficiency
Untreated blood clots in the legs can damage vein valves, leading to chronic venous insufficiency. This condition impairs blood flow back to the heart, causing swelling, pain, and skin changes.
- Symptoms:
- Swollen legs and ankles
- Aching or heaviness in the legs
- Itchy or flaky skin
- Open sores or ulcers
Importance of Early Intervention
The risks associated with untreated blood clots highlight the need for early diagnosis and proper treatment. Recognizing symptoms and seeking medical advice can prevent these life-threatening complications.
Regular check-ups, especially for those at higher risk, can help detect blood clots early and reduce the chances of serious health issues. Early intervention remains the most effective way to avoid severe problems related to blood clotting and ensure better health outcomes.
FAQs
Q1: What are the first signs of a blood clot?
Ans: The early symptoms of a blood clot depend on its location. For clots in the legs (deep vein thrombosis or DVT), signs include swelling, pain, tenderness, and warmth in the affected area.
If a clot travels to the lungs (pulmonary embolism or PE), symptoms may include sudden shortness of breath, chest pain, and a rapid heartbeat. Recognizing these clot symptoms early can help prevent serious complications.
Q2: Can dehydration cause blood clots?
Ans: Yes, dehydration can increase the risk of blood clots. When the body lacks adequate fluids, blood thickens, making it more likely to clot. Staying properly hydrated helps maintain smooth blood flow and reduces the chances of developing a clot.
Q3: How long does it take for a blood clot to form?
Ans: How long does it take for a blood clot to form depends on various factors, such as immobility, injury, or underlying medical conditions. A blood clot can form within hours to days of reduced movement or trauma. For example, clots can develop during long flights, after surgery, or when bedridden for extended periods.
Q4: Are blood clots common after surgery?
Ans: Yes, blood clots are a known risk after surgery, particularly orthopedic procedures like hip or knee replacements. Surgery can damage blood vessels, and post-operative immobility slows circulation, increasing the chance of clot formation. Doctors often recommend blood thinners or compression stockings to lower this risk.
Q5: Can blood clots go away on their own?
Ans: Some small blood clots may dissolve naturally as the body breaks them down. However, larger clots or those in critical areas, like the lungs or brain, require medical treatment. Ignoring a blood clot can lead to severe complications, so it’s essential to consult a doctor if you suspect one.
Q6: What foods help prevent blood clots?
Ans: Certain foods can support healthy blood flow and reduce blood clot risk.
- Leafy greens like spinach and kale provide nutrients that regulate clotting.
- Garlic and onions have natural blood-thinning properties.
- Berries and citrus fruits are rich in antioxidants that protect blood vessels.
- Omega-3 fatty acids in fish like salmon help lower inflammation and promote circulation.
Maintaining a balanced diet, along with staying hydrated, can aid in preventing blood clots.
Q7: How does flying increase blood clot risk?
Ans: Long flights increase the risk of blood clots due to prolonged inactivity. Sitting for extended periods slows blood flow, particularly in the legs, leading to potential clot formation. This condition, often called “economy class syndrome,” highlights why it’s important to stretch, walk, and stay hydrated during flights.
Q8: Can daily exercise help prevent clots?
Ans: Yes, regular exercise promotes healthy blood circulation, reducing the risk of blood clots. Activities like walking, swimming, or cycling help keep the blood moving, especially in the legs. Even simple leg stretches or foot movements during long periods of sitting can make a significant difference in preventing blood clots.
Q9: What is the difference between DVT and PE?
Ans: Deep vein thrombosis (DVT) is a blood clot that forms in a deep vein, typically in the legs. If part of this clot breaks free and travels to the lungs, it causes a pulmonary embolism (PE), which can block blood flow and become life-threatening. While DVT can cause leg pain and swelling, PE often presents with chest pain, shortness of breath, and rapid heart rate.
Q10: How do blood thinners work to prevent clots?
Ans: Blood thinners, or anticoagulants, reduce the blood’s ability to clot, helping prevent existing clots from growing and stopping new ones from forming. They don’t dissolve clots but lower the risk of complications like pulmonary embolism. Regular monitoring is often necessary to ensure proper dosage and minimize side effects.
Conclusion
Taking steps to avoid blood clots is essential for maintaining long-term health. Simple habits like staying active, maintaining a balanced diet, and staying hydrated can help prevent blood clots from forming. Regular movement, especially during long flights or extended periods of sitting, plays a key role in reducing risks.
For those at higher risk, medical guidance is essential. Routine check-ups, including a blood test for blood clots, can help detect issues early. In cases where preventive measures are not enough, treatments such as blood thinners or compression stockings provide additional protection.
Understanding the warning signs and seeking medical advice when needed can prevent serious complications like deep vein thrombosis (DVT) or pulmonary embolism. If you have risk factors, consulting a healthcare professional about how to avoid blood clots is the best way to protect your health. Proactive steps today can help prevent life-threatening conditions in the future.

