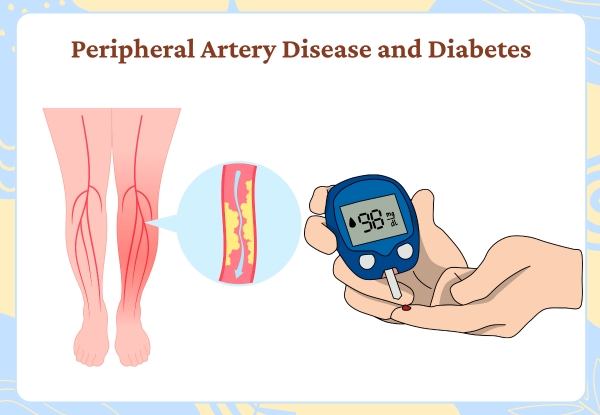
Peripheral Artery Disease and Diabetes are closely connected, with one condition increasing the risk and severity of the other. Many people with diabetes are unaware of how it affects blood circulation, particularly in the legs and feet, until it leads to serious health issues.
Understanding this connection is vital for early detection and timely action. This article breaks down the relationship between both conditions, outlines the signs to look out for, and shares useful guidance on prevention and treatment.
What Is Peripheral Artery Disease?

Peripheral Artery Disease, commonly known as PAD, occurs when the blood vessels outside the heart and brain narrow. It mainly affects the arteries that supply blood to the legs and feet. This condition results from fatty deposits, known as plaque, building up on the artery walls. Over time, this slows blood flow and causes discomfort during walking or physical activity.
Common Symptoms:
- Pain or cramping in the legs, especially after walking
- Numbness or weakness in the legs
- Coldness in the lower legs or feet
- Sores that heal slowly or not at all
- Colour changes in the skin of the legs
How Diabetes Increases PAD Risk

People with diabetes have consistently high blood sugar levels. This damages the lining of blood vessels, making it easier for plaque to develop and harder for the body to repair damage. Additionally, diabetes reduces the body’s ability to sense foot injuries due to nerve damage.
Key Factors That Link the Two Conditions:
- Damaged blood vessels due to high glucose levels
- Increased inflammation in the arteries
- Lower ability to fight infections
- Reduced blood circulation in limbs
This is why it’s vital to monitor the health of your feet and legs regularly if you are living with diabetes.
Why Early Diagnosis Matters
The combination of Peripheral Artery Disease and Diabetes can silently progress for years. Many patients only notice when the condition has reached an advanced stage. Early detection through medical tests can help prevent more serious outcomes, such as ulcers, infections, or in extreme cases, amputation.
Visiting the best diagnostic centre can make a big difference. A simple test like the Ankle-Brachial Index (ABI) can measure blood pressure in the ankle and arm to check for reduced circulation.
Treatment Options for Peripheral Artery Disease and Diabetes

Treatment usually includes a mix of lifestyle changes, medical management, and sometimes procedures. Each patient may require a different approach, depending on the severity of the condition and the presence of diabetes-related complications.
Standard Treatment Approaches:
- Medications
- To manage blood sugar, blood pressure, and cholesterol
- To improve blood flow and prevent clotting
- To manage blood sugar, blood pressure, and cholesterol
- Lifestyle Changes
- Stopping smoking
- Healthy eating with a focus on blood sugar control
- Regular walking and leg-focused activity
- Stopping smoking
- Specialist Procedures
- Angioplasty (opening blocked arteries)
- Bypass surgery (rerouting blood flow)
- Endovascular therapy (minimally invasive options)
- Angioplasty (opening blocked arteries)
A peripheral artery disease specialist will guide which approach suits best, based on test results and health history.
Prevention: Lowering Your Risk with Everyday Habits
If you have diabetes, taking extra care can reduce your risk of PAD. Prevention starts with making better choices daily.
Practical Tips to Prevent PAD:
- Keep blood sugar within recommended levels
- Maintain healthy blood pressure and cholesterol
- Check your feet every day for cuts or sores
- Walk daily to improve circulation
- Visit your doctor regularly for foot and leg checks
By following these steps, it’s possible to delay or even avoid the complications associated with Peripheral Artery Disease and Diabetes.
Choosing the Right Care Team
Picking the right healthcare team is essential. Look for:
- A clinic experienced in managing both diabetes and vascular conditions
- Access to advanced diagnostic tools
- Personalised treatment plans
- Support for lifestyle coaching and diet
A trusted centre like Midas Care Clinic, known for its track record in PAD care, can give you confidence that you’re on the right path.
FAQs
Q1. What is the connection between peripheral artery disease and diabetes?
Answer: Diabetes causes high blood sugar, which damages blood vessels. This damage increases the risk of narrowed arteries, leading to PAD.
Q2. Can I prevent PAD if I already have diabetes?
Answer: Yes, through healthy eating, regular activity, not smoking, and regular foot checks. Early screening helps too.
Q3. What are early signs of PAD in diabetics?
Answer: Look for leg pain while walking, cold feet, discolouration, or wounds that don’t heal. These can all be early warning signs.
Q4. Is PAD in diabetics serious?
Answer: Yes. It raises the risk of ulcers, infections, and even amputation if not managed in time.
Q5. How is PAD diagnosed?
Answer: A simple test called the Ankle-Brachial Index compares blood pressure in the ankle and arm. Imaging tests may also be used.
Q6. Can lifestyle changes alone help?
Answer: In mild cases, yes. Walking, healthy food, quitting tobacco, and blood sugar control all make a big difference.
Q7. How often should diabetics get checked for PAD?
Answer: At least once a year or more frequently if symptoms appear.
Q8. Where can I find help for PAD and diabetes?
Answer: Specialised clinics such as Midas Care Clinic and top-rated diagnostic centres provide dedicated support.

