Deep vein thrombosis, or DVT, is a condition where a blood clot forms in a deep vein, usually in the leg. It can cause swelling, pain, and if left untreated, may lead to serious health risks like pulmonary embolism. Early diagnosis and treatment can help prevent complications.
Introduction
If you’ve heard of deep vein thrombosis but aren’t sure what it actually means, you’re not alone. Many people come across the term during a medical check-up, after surgery, or while reading about leg pain and swelling online. It’s a condition that might sound complex, but understanding it is important especially because it can lead to serious complications if ignored.
People usually search for this topic when they notice symptoms like unusual leg pain, swelling, or changes in skin colour. Some might be looking for prevention tips, others may be worried after a long flight or hospital stay. No matter the reason, knowing what deep vein thrombosis is and how it works can help you make informed decisions about your health.
This guide is written to give you clear, practical information without medical jargon so you know what to watch out for and when to act. Whether you’re concerned for yourself or someone close to you, being aware of the signs and causes of DVT can make a real difference.
What is Deep Vein Thrombosis?
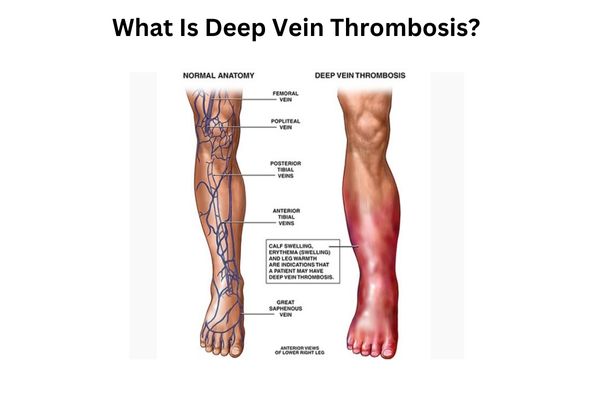
Deep vein thrombosis, often shortened as DVT, happens when a blood clot forms in one of the deep veins of the body, usually in the legs. The DVT full form stands for deep vein thrombosis, which simply refers to a blockage inside a deep vein.
To understand it in simpler terms, imagine your veins as smooth pathways that help carry blood back to your heart. When everything is working well, blood flows without any issue. But sometimes, a clot can form and stop that flow. When this happens in a deep leg vein, it can cause swelling, pain, or a warm feeling in the area.
Inside your body, this clot isn’t just sitting there quietly. It can grow and put pressure on the surrounding tissue. In more serious situations, part of the clot might travel through the bloodstream and reach the lungs, which leads to a condition called pulmonary embolism, a medical emergency.
DVT affects the circulation system, especially in the leg veins, and if left untreated, it can lead to long-term complications. But when identified early, it can often be managed with proper care and medication.
Understanding how deep vein thrombosis works gives you a better idea of what’s really happening beneath the surface when symptoms appear. It also shows why even a small change in how your legs feel shouldn’t be ignored.
How DVT Develops in the Body
When a blood clot forms deep inside the veins, it doesn’t just appear out of nowhere. The process begins gradually and is often triggered by changes in how blood flows or how the blood itself behaves.
Here’s a clear breakdown of how deep vein thrombosis develops inside the body:
- Slowed or reduced blood flow
In some situations, such as sitting for long hours without moving, the blood in the legs doesn’t flow as freely. This can happen during long flights, car rides, or after surgery. When the movement of blood slows down, there’s a higher chance that a clot forms. - Damage to the vein wall
A direct injury to a vein like a fracture, a bump during an accident, or even certain surgeries can disturb the normal lining of the vessel. When that lining is irritated or broken, it can trigger the body to start forming a clot as a repair mechanism. - Changes in blood composition
Certain health conditions, medications, or inherited disorders can make the blood more likely to clot. In some people, their blood naturally contains higher levels of clotting proteins. This can quietly raise the risk without them knowing. - Extended periods of inactivity
Being in bed due to illness, recovering from an operation, or even working long hours at a desk can lead to vein blockage. Without regular muscle movement, blood doesn’t get pumped back up to the heart efficiently. - Underlying medical conditions
Conditions like cancer, heart disease, and autoimmune disorders can all affect how blood circulates. Some treatments for these illnesses may also contribute to clot formation in the deep veins.
Facts and Data:
- According to the U.S. Centers for Disease Control and Prevention (CDC), up to 900,000 people in the United States are affected by DVT and pulmonary embolism each year.
- Nearly 1 in 10 hospital deaths are related to blood clots like deep vein thrombosis, many of which are preventable with early care.
- Long flights lasting more than 8 hours to 10 hours can double the risk of DVT in susceptible individuals, especially when seated without movement for extended periods.
- Studies show As many as half of those who get a deep vein thrombosis may experience long-term complications in the affected leg if not treated early.
This internal process explains why deep vein thrombosis often develops silently and highlights the importance of recognising risk factors early.
Common Symptoms of DVT
Recognising the signs of deep vein thrombosis early can make a real difference. While some people may not notice any symptoms at all, others may feel unusual discomfort in their legs that gradually becomes more noticeable.
Here are the most common DVT symptoms to be aware of:
- Persistent leg pain
This often begins in the lower leg and might feel like a cramp or a steady ache. The pain can become worse when walking or standing for long periods. - Swelling in the calf or thigh
One leg may appear visibly swollen while the other remains normal. This is due to a blood clot obstructing flow, causing fluid to collect in the tissues. - Tenderness in a specific spot
Gently pressing the affected area particularly the back of the calf may cause discomfort. This tenderness can feel different from muscle soreness. - Warm skin over the clot area
The skin might feel warmer than the surrounding areas, often accompanied by redness. It may also appear tight or stretched due to the swelling. - Discolouration or redness
Some people notice a change in skin colour around the affected area, usually becoming reddish or bluish.
Areas Most Commonly Affected
- Calf: This is the most frequent site where clots form. People often dismiss the discomfort here as minor muscle strain.
- Thigh: DVT higher up in the leg may feel deeper and more diffused.
- Pelvic veins: Though less common, clots in these veins can still produce symptoms in the lower abdomen, buttocks, or thighs.
When to Take It Seriously
Some symptoms may seem mild in the beginning, but if they appear suddenly or worsen, they should never be ignored. Signs that call for urgent attention include:
- Swelling in one leg without any injury
- Pain that doesn’t go away or gets worse over time
- Skin that feels warmer than usual, especially in the lower leg
- Sudden shortness of breath (this could mean the clot has moved to the lungs)
Early Stage DVT Symptoms in the Leg
In the beginning, deep vein thrombosis may not feel serious. The symptoms often show up in quiet ways that many people overlook. These early signs are important to notice before a full vein blockage occurs.
Here are some of the early stage DVT symptoms leg:
- A dull ache in the calf or thigh, often confused with simple muscle fatigue
- Minor leg swelling, usually on one side, that doesn’t go away with rest
- A feeling of tightness in the leg, even without visible changes
- Mild warmth or discolouration in the skin that gradually becomes more noticeable
- Slight pain while walking or flexing the foot
These early warning signs of DVT in the leg are subtle but can be the body’s first alert. Acting on them early can help avoid complications later.
Main Causes Behind Deep Vein Thrombosis
There’s no single cause behind deep vein thrombosis. Instead, it develops when several risk factors combine and affect the normal flow of blood. Knowing what increases your chances can help you take the right steps early on.
Here are some of the most common DVT causes:
- Prolonged immobility
Sitting or lying down for long hours, especially during prolonged bed rest, recovery from surgery, or long-distance travel, can slow down blood flow in the legs. This sets the stage for clot formation. - Major surgeries or physical trauma
Orthopaedic procedures, abdominal surgeries, or injuries that damage blood vessels can trigger clotting as the body attempts to heal. - Certain medical conditions
Cancer, heart disease, and autoimmune disorders may affect how blood clots. People with these conditions are often at higher risk. - Family history of clotting disorders
Genetics can play a role. If a close family member has had deep vein thrombosis, your chances of developing it may be higher. - Hormone-related medications
Birth control pills, hormone replacement therapy, or certain fertility treatments can increase clotting tendencies, especially when combined with other risk factors. - Pregnancy and postpartum period
The added pressure on veins in the pelvic region and hormonal shifts during pregnancy can increase the chance of a blood clot forming. - Being overweight or obese
Extra weight puts more pressure on the leg veins, which can make it harder for blood to circulate efficiently.
Understanding these factors allows you to recognise when you’re in a higher-risk situation. Whether it’s preparing for a hospital stay or planning a long flight, being aware of what causes deep vein thrombosis helps you act sooner.
Who is at Risk of Developing DVT?
While deep vein thrombosis can affect anyone, certain groups of people are more likely to develop it. Understanding who falls into a high risk group helps in recognising early signs and taking preventive steps.
Here’s a breakdown of people more prone to blood clots and who gets DVT most often:
- Older adults
As we age, blood flow may slow down, and the veins become less flexible. People over 60 are at greater risk, especially if they have other health conditions. - Pregnant individuals and new mothers
Pregnancy increases pressure on the pelvic veins. The risk remains high during the weeks after delivery due to hormonal changes and reduced mobility. - People living with obesity
Excess body weight places added pressure on the veins in the legs, which can affect normal circulation and increase the risk of clotting. - Smokers
Smoking affects the health of blood vessels and increases clotting tendencies. When combined with other risks like age or hormone therapy, the chance of developing DVT rises. - Those with a sedentary lifestyle
Limited movement from a desk job, chronic illness, or lack of physical activity can cause blood to pool in the lower limbs. Over time, this leads to an increased risk. - Frequent flyers and travellers
Long flights or road trips where legs stay still for hours can increase the chance of a blood clot forming. Sitting in the same position restricts circulation, especially in the lower body. - People with certain medical conditions
Cancer, heart failure, or inherited clotting disorders can raise the chance of deep vein thrombosis, even in younger individuals.
Being aware of these risk factors helps you stay alert. Whether it’s planning a trip or managing a health condition, knowing where you stand in terms of risk allows you to take timely action.
How DVT is Diagnosed
When a doctor suspects deep vein thrombosis, they rely on specific tests to confirm if a blood clot is present. Diagnosis plays a key role in preventing complications like pulmonary embolism or long-term leg damage.
Here are the most common ways DVT is diagnosed:
- Doppler ultrasound
This is the most widely used test. It uses sound waves to check blood flow in the veins. If there’s a blockage or clot, the flow appears different. The test is painless and often takes less than 30 minutes. - D-dimer blood test
This test checks for a substance in the blood that increases when a clot forms. While a high result doesn’t confirm DVT on its own, it helps doctors decide if further testing is needed. - Venography
Though rarely used, this test involves injecting a contrast dye into a vein and taking X-rays to locate the clot. It may be done when ultrasound results are unclear. - MRI or CT scans
These are used in certain cases where clots are suspected in areas beyond the legs, such as the pelvis. They provide detailed imaging for complex cases.
What to Expect at a Diagnostic Center
When you visit a center for diagnostic tests for DVT, you can expect a brief medical history review followed by one or more of the above tests. There’s no special preparation required in most cases. The testing team may ask about symptoms, recent travel, or any ongoing medications.
For individuals seeking deep vein thrombosis treatment in Mumbai, it’s essential to choose a facility that offers same-day testing and access to a vascular specialist. The Best diagnostic center in Vasai will usually have Doppler ultrasound and D-dimer testing on-site, along with physicians experienced in managing DVT cases.
Timely diagnosis ensures the right treatment starts early, reducing the risk of further complications. If you notice signs like unexplained swelling or leg pain, getting tested promptly is always the best step forward.
What Happens if DVT is Left Untreated?
Deep vein thrombosis is more than just a blood clot in the leg. If it’s not diagnosed and treated in time, the consequences can be serious, even life-threatening. The body doesn’t always break down clots on its own, which is why medical care is essential.
Here are the possible blood clot complications when DVT is left untreated:
- Pulmonary embolism (PE)
This is the most severe risk. If the blood clot breaks off and travels to the lungs, it can block a major artery. This restricts oxygen flow, causes sharp chest pain, and may lead to shortness of breath. In some cases, it can be fatal. - Post-thrombotic syndrome (PTS)
Over time, the clot can damage the valves in the vein. This leads to long-term problems such as chronic leg pain, swelling, and heaviness. Some people also develop skin discolouration or ulcers. - Permanent vein damage
Ongoing inflammation caused by the clot can scar the vein walls. This reduces flexibility and affects how well blood flows through the affected limb. - Increased risk of future clots
Once someone has had DVT, the chances of another episode are higher. Without treatment, the risk of repeated clotting becomes more difficult to manage. - Delayed diagnosis of other conditions
Some people assume their pain is due to muscle strain or varicose veins. Ignoring the signs can lead to a missed opportunity for timely care and allow the clot to grow.
Leaving DVT untreated isn’t just about discomfort. It’s about the real danger of the clot travelling or causing lasting damage. Understanding these outcomes helps reinforce why early diagnosis and proper treatment are so important.
Can DVT be Prevented?
Yes, in many cases, deep vein thrombosis prevention is possible by making small changes to your daily routine. While not all risk factors can be controlled, understanding how to reduce them is a strong step forward.
Here are some everyday habits that help with how to avoid blood clots:
- Stay active and move regularly
Avoid sitting still for long stretches. Stand up, stretch, or walk every one to two hours, especially during flights, road trips, or desk jobs. - Keep your body hydrated
Drinking enough water keeps the blood from thickening, especially during travel or hot weather. Dehydration can slow circulation and raise clot risk. - Wear compression stockings when advised
These help maintain steady blood flow in the legs and are often recommended after surgery, during long trips, or if you’ve had DVT before. - Watch your posture while sitting
Crossing your legs or letting them hang without support can reduce blood flow. Keeping your legs uncrossed and feet flat helps maintain better circulation. - Exercise regularly
Simple leg exercises or walking every day helps keep the calf muscles active. These muscles play a key role in pumping blood back toward the heart. - Lose excess weight if needed
Reducing pressure on your leg veins can lower your risk, particularly if obesity is a contributing factor. - Stop smoking
Smoking affects how blood clots and damages blood vessel walls. Quitting is one of the most effective long-term steps you can take.
When to Consider Medical Prevention
In some cases, lifestyle changes might not be enough, especially for those with higher risk due to medical conditions or recent surgeries. Doctors may recommend:
- Blood-thinning medication (anticoagulants), often given after surgery or while being treated for cancer
- Temporary use of compression devices, particularly after hospital stays
- Pre-travel precautions, including wearing compression gear or walking regularly during long trips, to prevent DVT while traveling
If you’ve had DVT before, or your doctor believes you’re at risk, preventive steps should always be part of your care plan. Early prevention is not just about comfort, but about protecting your long-term health.
When to See a Deep Vein Thrombosis Specialist
Sometimes it’s easy to dismiss pain or swelling in the leg as something minor. But there are certain signs you should never ignore. Knowing when to consult a deep vein thrombosis specialist can protect you from serious complications and guide you toward the right care.
Here are the signs that suggest it’s time to seek medical advice without delay:
- Sudden or increasing swelling in one leg, especially if it’s accompanied by tenderness or redness
- Sharp pain in the calf or thigh that gets worse when walking or standing
- Warmth in the leg, or skin that feels unusually tight and stretched
- Shortness of breath, chest pain, or light-headedness, which may signal the clot has moved to the lungs
In these situations, medical evaluation becomes urgent. Diagnosis and treatment should not be postponed.
If you’re experiencing any of these symptoms, visiting a clinic with experience in vascular health is essential. At Midas Care Clinic, you can consult Dr Chandrakant, a recognised deep vein thrombosis specialist who understands the urgency of such cases and provides personalised treatment based on your condition.
Getting timely help not only improves your recovery but also prevents future complications like post-thrombotic syndrome or pulmonary embolism. When symptoms show up, listening to your body and acting early makes all the difference.
Conclusion
Deep vein thrombosis isn’t always easy to spot, but it should never be taken lightly. A blood clot forming in the leg can lead to serious complications if ignored, and that’s why early awareness is so important. From understanding the signs to knowing when to seek help, being informed puts you in control of your health.
Whether it’s recognising subtle leg discomfort or learning how to prevent clots during long travel or recovery, the steps you take now matter. If you’re experiencing symptoms or fall into a higher-risk group, don’t wait to speak with a professional.
If you’re looking for personalised care and reliable guidance, Midas Care Clinic offers expert consultation through Dr Chandrakant, a trusted deep vein thrombosis specialist. Timely action can make all the difference in your recovery and overall well being.
Stay alert to what your body is telling you. When it comes to DVT, early steps are often the safest ones.
Frequently Asked Questions
Q1: What does DVT pain feel like?
Ans: Pain from deep vein thrombosis often begins as a dull ache or tightness, usually in the calf or thigh. It may feel like a cramp that doesn’t go away, and walking or standing can make it worse.
Q2: Can DVT go away on its own?
Ans: While some clots may shrink naturally, most require medical care to avoid complications. Ignoring DVT symptoms increases the risk of serious conditions like pulmonary embolism.
Q3: How long does DVT last?
Ans: With timely DVT treatment, symptoms can improve within a few weeks. However, complete recovery may take several months, especially if swelling or discomfort lingers.
Q4: Is DVT life-threatening?
Ans: Yes, if not treated in time. A clot can travel to the lungs and block blood flow, leading to a condition called pulmonary embolism. This makes early diagnosis and treatment crucial.
Q5: Can I walk with DVT in my leg?
Ans: Movement is usually encouraged under a doctor’s guidance. Walking helps improve circulation, but any activity should be discussed with your specialist first.
Q6: How is DVT confirmed by doctors?
Ans: Doctors use tools like Doppler ultrasound and D-dimer blood tests. If you’re in Mumbai, a trusted diagnostic center in Mumbai such as Midas Care Clinic offers both testing and expert consultation.
Q7: What are the chances of DVT recurring?
Ans: Once you’ve had deep vein thrombosis, your risk of recurrence increases, especially without lifestyle changes or follow-up care. Long-term management can help reduce that risk.
Q8: Is DVT more common in one leg?
Ans: Yes, DVT typically affects one leg. It’s often the left leg due to how blood flows from the lower body, but either leg can be affected depending on the cause.
Q9: Do I need surgery for DVT?
Ans: Most cases don’t require surgery. DVT treatment usually includes medication, compression therapy, and lifestyle adjustments. Surgery is considered only for severe or life-threatening situations.
Q10: What foods or habits can help reduce clot risk?
Ans: Staying hydrated, avoiding long periods of sitting, quitting smoking, and keeping a healthy weight can lower your risk. A diet rich in leafy greens, omega-3s, and low in processed food may also help support vascular health.

